Prior authorization
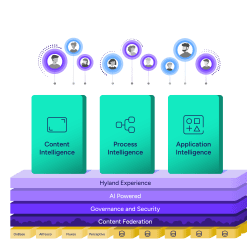
Speed response times with AI-powered intelligent document processing. Easily capture, classify and extract data for prior authorization reviews.
Optimize processes to adhere to the Centers for Medicare & Medicaid Services rules and avoid penalty fines.
Effectively track and report on compliance with prior authorization requirements.
Reduce the risk of a PHI breach by eliminating the manual processing of sensitive and private information.