Improving eligibility verification with AI
Hyland Insurance Card Extraction helps prevent payer claim denials.

Registration and eligibility verification is the biggest reason for the denial of payer claim payments. That’s why accurately capturing data from insurance cards is essential for checking patient eligibility and preventing lost revenue.
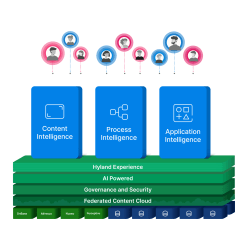
Hyland Insurance Card Extraction uses optical character recognition and machine learning technology to automate the process of collecting patient data from scanned insurance cards. The extracted patient data is then sent to Epic or routed to a review team.
Discover how this Hyland solution can save your staff time, prevent rekeying errors and ensure accurate data for payer eligibility verification.
You might also like:

Great Ormond Street Hospital
Leading pediatric hospital streamlines clinical workflows to improve the patient experience by digitizing consent forms, signature capture and use of clinical guidelines.

What is case management?
Case management is a collaborative approach to managing cases or projects that involve multiple stakeholders and require extensive documentation and tracking.

Sharp HealthCare
Healthcare group automates 150 workflows and unites content for use in EHR, ERP and core systems with Hyland.

Hyland’s 2024 Q1 releases include key enterprise platform updates
Take advantage of the latest Hyland solution updates, including key enterprise platform updates, as well as new and enhanced solutions for healthcare and AP.