Transforming key payer processes with intelligent automation
This whitepaper from HIMSS and Hyland examines how payer organizations can work smarter and more efficiently.
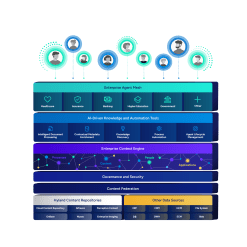
Harness the power of a unified content, process and application intelligence platform to unlock the value of enterprise content.
Learn more
Automate your document-centric processes with AI-powered document capture, separation, classification, extraction and enrichment.
Learn about Hyland IDPIt's your unique digital evolution … but you don't have to face it alone. We understand the landscape of your industry and the unique needs of the people you serve.
 Overview of industries
Overview of industries
Countless teams and departments have transformed the way they work in accounting, HR, legal and more with Hyland solutions.
 Overview of departments
Overview of departments
We are committed to helping you maximize your technology investment so you can best serve your customers.
 Overview of services
Overview of services

Learn proven strategies, connect with experts, innovate boldly
Register for CommunityLIVE 2026 today
Our exclusive partner programs combine our strengths with yours to create better experiences through content services.
Overview of partners
Join The Shift newsletter for the latest strategies and expert tips from industry leaders. Discover actionable steps to stay innovative.
Register now
Hyland connects your content and systems so you can forge stronger connections with the people who matter most.
Learn about HylandWith our modern, open and cloud-native platforms, you can build strong connections and keep evolving.
 Dig deeper
Dig deeper
Reading time minutes
This whitepaper from HIMSS and Hyland examines how payer organizations can work smarter and more efficiently.

Rising drug prices, inflation and workforce shortages are adding up to increasing expenses for healthcare payers.
To contain growing costs, payers need to be more efficient with the vast amounts of data that health plans manage. That makes intelligent automation a game-changer.
This whitepaper from HIMSS and Hyland examines the use of automation technologies and AI to anticipate users’ needs and streamline manual processes.
Explore how intelligent automation can:
You’ll also learn how one of the largest provider-sponsored health plans in the U.S. significantly reduced costs and made its processes more efficient with automation.



