Why unstructured data in healthcare matters
Unstructured data in healthcare is a critical problem because it is a key part of a patient’s overall medical history. Examples of unstructured data include things like clinical documents and charts, clinical narratives, lab results, consents, referral documents and a wealth of medical images — even images from digital cameras, smartphones and scopes.
If this vital unstructured information is not included in the core clinical systems healthcare providers use every day, then the patient picture is woefully incomplete. In fact, industry estimates from analysts such as Gartner and IDC state that, even today, nearly 80% of the information that exists on a patient is in an unstructured format.
The providers themselves seem aware of the problems this unstructured data causes, especially when it comes to medical images. For example, 90% of the HIMSS study respondents stated it was critical or very important for clinicians to have access to patient images at the point of care. However, they also stated an average of 18% of their images are captured offline (e.g., encounter-based, via mobile device, etc.). And 65% of respondents cited a direct integration with their radiology picture archiving and communication system (PACS) was their primary means of integrating medical images with their EMR. This leaves a potentially vast array of non-radiology images inaccessible from this core clinical system.
When unstructured content and images aren’t included in the IT systems that are central to interoperable infrastructures, then these interoperability efforts are incomplete.
Harnessing unstructured content for true health IT interoperability
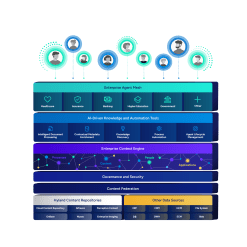
Considering the importance of unstructured content in creating a comprehensive patient record, how can this information be harnessed to ensure it’s included in interoperability initiatives? While definitely a complex undertaking, the process can be boiled down to the following three steps:
#1: Identify
First, you need to identify where your valuable unstructured data resides. Often this information exists in multiple departmental content management systems, third-party cloud archives, paper medical documents and charts, faxes, email, specialty imaging systems, isolated modality stations, mobile devices, physical storage media and more.
#2: Consolidate
Next, steps need to be taken to consolidate this data as much as possible. Consolidate electronic documents from existing repositories and scan, index and archive paper documents into a single repository. For medical imaging, enterprise imaging solutions such as a vendor neutral archive, universal image viewer and image connectivity tools can be implemented to complement or replace some PACS. This approach enables centralized management, access and sharing of all types of images — regardless of format and source. It also eliminates vendor lock and block that often accompanies proprietary systems, giving organizations all-encompassing ownership and control of their imaging data. These content services and enterprise imaging repositories can be consolidated further by establishing a single enterprise platform with a shared storage and presentation (i.e., viewing) layer.
#3: Connect
Finally, these consolidated repositories need to be integrated with core clinical systems such as the EMR. Do this by using accepted industry standards such as HL7, Fast Healthcare Interoperability Resources (FHIR), DICOM, Cross Document Sharing (XDS) and more. The goal is to present unstructured and structured patient data in a single view that clinicians can access within their workflow via the EMR throughout the enterprise and beyond.
If done well, you’ll take interoperability to the next level by sharing complete patient information for improved care decisions.
> Learn more | HIMSS Market Insights on improving connected care and advancing interoperability goals
This post was originally published on himssconference.org.