Intelligent capture for digitizing medical records
Automation is a prerequisite to delivering patient-centered care in the post-HITECH era.
Automation is a prerequisite to delivering patient-centered care in the post-HITECH era.

The Health Information Technology for Economic and Clinical Health (HITECH) Act and the Meaningful Use incentives that stemmed from it have had a significant impact on the adoption of electronic health record (EHR) systems by healthcare organizations.
According to HealthIT.gov, 96% of all non-federal acute care hospitals now use EHR technology. That figure, as of 2021, marked a substantial increase from a decade earlier, when only 28% of such hospitals had adopted an EHR.
So that means paper is a thing of the past in healthcare, right? Hardly. Despite the move toward digitization, paper is still a fixture in all corners of a healthcare enterprise — especially in the health information management (HIM) department.
Before EHRs gained widespread use, paper medical charts were the norm. Many of these historical charts continue to be stored and maintained by health systems for compliance purposes.
In addition, just because a hospital leverages EHR technology doesn’t mean it extends to every aspect of the facility’s clinical operations. It also has no bearing on the paper practices of that hospital’s care partners.
According to IDC, the top reasons hospitals, clinics and healthcare organizations keep using paper include:
Yes, paper is still a reality in healthcare — and a costly one at that — from a monetary and quality-of-care perspective. Paper is also a key contributing factor to the astronomical administrative costs that inflate U.S. healthcare spending. Research shows that administrative costs account for 15% to 30% of medical spending.
While significant, the monetary costs of managing paper may actually be the lesser of two evils for some hospitals. Maintaining disparate paper and electronic records for the same patient can lead to a fragmented medical history that can impact clinical decision-making and care.
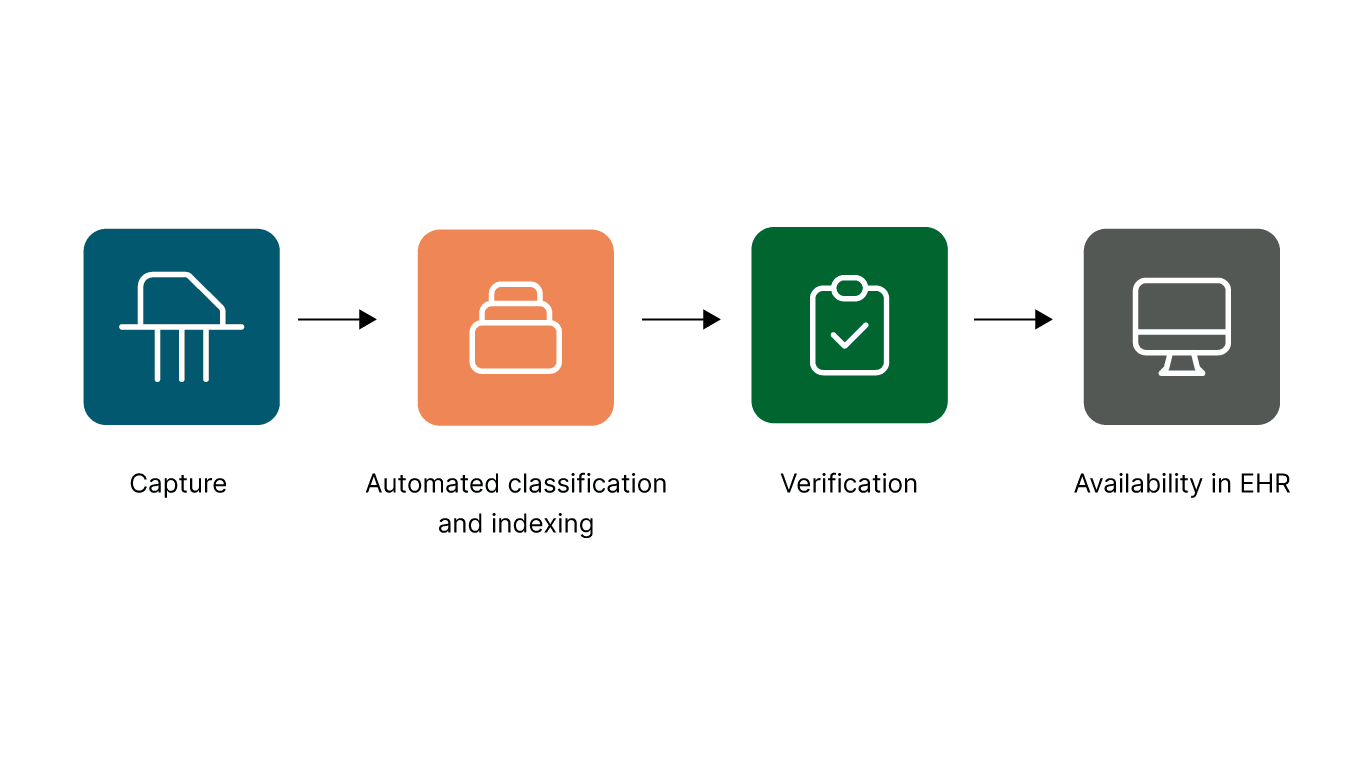
Health systems realize the importance of digitizing paper healthcare documents and getting this information into the EHR. In most instances, this effort falls to the HIM department as part of its responsibly for maintaining the legal medical record at a hospital or healthcare organization. The problem is the digitization practices employed by these healthcare facilities often are laborious, time-consuming and error prone.
For example, digitization requires manual sorting, batching and scanning. Some healthcare facilities even manually index and classify documents (according to document type, patient and visit). It takes a human an average of 40 seconds to read and determine what a medical document is, let alone manually enter indexing information. These manual processes are also highly susceptible to human error. Finally, the HIM department usually reviews each scanned document for quality assurance (QA) prior to making it available in the EHR.
> Read more | Intelligent MedRecords: Improve the speed and accuracy of HIM tasks
Intelligent data capture and document classification solutions are available to help automate many of the manual steps that can bog down the digitization process. Intelligent data capture solutions can capture, process and transform virtually any type of paper-based or digital document into useful and actionable information. By leveraging pattern-based recognition algorithms, these systems can learn from multiple data sets to continuously improve their accuracy and performance.
Intelligent data capture and extraction can be used to streamline the indexing process by automatically populating key indexing fields. Similarly, intelligent document classification technology helps automate the process of identifying and categorizing key document types. These solutions use optical character recognition (OCR) and pattern-based logic to automatically classify medical documents by identifying the key content characteristics (keywords, semantics, document layout, etc.). Any documents that can’t be confidently identified by the software are placed in a folder for manual exception processing.
Intelligent classification technology can identify medical documents in as little as five seconds, as opposed to the 40 seconds it takes humans. This accelerated workflow saves time and money while improving accuracy and consistency.
In addition to these process benefits, intelligent document classification also provides several operational efficiencies. For example, a streamlined classification workflow can help shorten patient length of stay, reduce labor costs and improve the visibility of patient information to improve clinical decisions and outcomes.
Perhaps most importantly, helping healthcare organizations slash the time they spend on medical records digitization gives staff members more time to devote to tasks that have a more direct impact on patient care and the overall patient experience.
— Tara Neitzel, IT operations manager, Sentara Healthcare

Facilitate the intake and completion of patient forms by automatically populating existing information and providing a user-friendly interface for additional data collection.
Hyland’s medical records classification provides the following benefits: