VNS Health
New York health plan enhances efficiency and security by automating appeals and grievances processes.
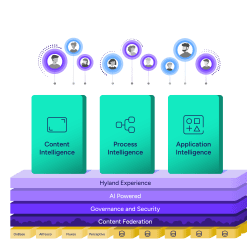
Harness the power of a unified content, process and application intelligence platform to unlock the value of enterprise content.
Learn more
Explore Hyland’s solutions by industry, department or the service you need.
Overview of solutionsIt's your unique digital evolution … but you don't have to face it alone. We understand the landscape of your industry and the unique needs of the people you serve.
 Overview of industries
Overview of industries
Countless teams and departments have transformed the way they work in accounting, HR, legal and more with Hyland solutions.
 Overview of departments
Overview of departments
We are committed to helping you maximize your technology investment so you can best serve your customers.
 Overview of services
Overview of services

Discover why Hyland is trusted by thousands of organizations worldwide.
Hear from our customers
Our exclusive partner programs combine our strengths with yours to create better experiences through content services.
Overview of partners
Find resources to power your organization's digital transformation.
Browse the resource center
Hyland connects your content and systems so you can forge stronger connections with the people who matter most.
Learn about HylandWith our modern, open and cloud-native platforms, you can build strong connections and keep evolving.
 Dig deeper
Dig deeper
Reading time minutes
New York health plan enhances efficiency and security by automating appeals and grievances processes.

The appeals and grievances (A&G) process can make or break the reputation of any healthcare payer. Efficient A&G management can elevate customer satisfaction, while slow responses and resolution can anger members and elicit noncompliance penalties.
While essential, bringing efficiency to A&G is easier said than done. Traditional A&G processes are paper-based and extremely manual, which can lead to lost documents and interrupted workflows that negatively impact turnaround times. VNSNY CHOICE Health Plans is very familiar with the obstacles that are often encountered during A&G processing and successfully addressed these issues with an automated solution from Hyland.
Back in 2016, VNSNY CHOICE used Access databases to track all of its A&G submissions and stored related correspondence and documents in Microsoft Windows folders.
VNSNY CHOICE knew there had to be a better way and began the search for a new solution. “Hyland’s solution stood out among the competition because the OnBase platform could be used in other areas of the company besides just A&G,” says Tanya McCray, vice president, Grievance and Appeals and Vendor Management, VNSNY CHOICE. “The demonstration they delivered also illustrated how user-friendly the system was as well as the personal touch their team provided clients.”
— Tanya McCray, Vice President, Grievance and Appeals and Vendor Management, VNSNY CHOICE
VNSNY CHOICE implemented OnBase in June 2016 and realized a number of benefits shortly thereafter. With the new system, A&G data is categorized by a third-party vendor based on incoming mail or email. This incoming information is then vetted by CHOICE staff and entered as cases for OnBase to auto assign. OnBase ingests membership and eligibility information and uses this data to automatically populate templates for the appropriate A&G response.
“Automatic case assignment and template population has helped cut a good 30 minutes out of the time it previously took to process each case,” says McCray.
The OnBase platform also helped address many of the issues VNSNY CHOICE experienced with the Access database. For example, case loads are easier to track since all necessary information is stored in the same system. Other advantages include the ability for staff to automatically generate a Centers for Medicare and Medicaid (CMS) universe and the ability to designate select data fields as required or fixed.
“With OnBase, our A&G data is cleaner and more secure,” says McCray. “We can trust what’s in there.”
Even prior to using Hyland, VNSNY CHOICE generated performance dashboards so it could visualize cases and identify trends. However, this process has been streamlined with OnBase. Users can now identify provider information and member complaint case types that match what regulators want reported more easily.
VNSNY CHOICE plans to make additional enhancements to its OnBase A&G solution going forward. Specifically, the payer has plans to integrate the system with other line-of-business applications so more data can be ingested and additional automated workflows can be initiated.
— Tanya McCray, Vice President, Grievance and Appeals and Vendor Management, VNSNY CHOICE