Mutual of Enumclaw
Regional insurer cuts claims processing times from days to hours.
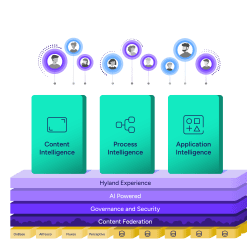
Harness the power of a unified content, process and application intelligence platform to unlock the value of enterprise content.
Learn more
Explore Hyland’s solutions by industry, department or the service you need.
Overview of solutionsIt's your unique digital evolution … but you don't have to face it alone. We understand the landscape of your industry and the unique needs of the people you serve.
 Overview of industries
Overview of industries
Countless teams and departments have transformed the way they work in accounting, HR, legal and more with Hyland solutions.
 Overview of departments
Overview of departments
We are committed to helping you maximize your technology investment so you can best serve your customers.
 Overview of services
Overview of services

Discover why Hyland is trusted by thousands of organizations worldwide.
Hear from our customers
Our exclusive partner programs combine our strengths with yours to create better experiences through content services.
Overview of partners
Find resources to power your organization's digital transformation.
Browse the resource center
Hyland connects your content and systems so you can forge stronger connections with the people who matter most.
Learn about HylandWith our modern, open and cloud-native platforms, you can build strong connections and keep evolving.
 Dig deeper
Dig deeper
Reading time minutes
Regional insurer cuts claims processing times from days to hours.

Mutual of Enumclaw (MoE), a regional mutual insurance company, struggled with an aging legacy claims system. It was a basic solution, minimally configurable and with limited functionality. “Things were missing,” said Jeff Obermeyer, claims business manager, Mutual of Enumclaw. “The solution’s diary systems were antiquated and users struggled to identify efficiencies due to system limitations. We were also missing the analytics component, or the ability to do scoring, see trouble areas, or find future opportunities, and we were having trouble allocating work to the right adjusters at the right time.” On top of it all, the legacy system vendor would soon stop support for the solution. “That represented a real risk,” said Obermeyer.
— Jeff Obermeyer, Claims Business Manager, Mutual of Enumclaw
To combat the challenge, MoE invested in Hyland's OnBase. From its earliest implementation, the content services platform bolstered MoE’s legacy system and allowed the insurer to accomplish previously impossible goals the legacy system.
That included a first notice of loss (FNOL) tool, which the insurer built within OnBase using WorkView, streamlining the process. The ability to use OnBase to create business rules allowed MoE to automate the FNOL process, accurately assigning certain claim types to the appropriate adjuster.
Previously, there was no formalized claim process. A call or email would arrive, a customer service representative would manually input information into an ACCORD form, and then it was printed and validated by hand. It was put in a bin, picked up by courier, scanned, and indexed without a claim number. Eventually it was printed again, rescanned, and emailed to a manager who would assign to an adjuster. Assigning a claim number alone could take a half day, if it was lost during the process. Now the entire process takes about four hours.
MoE also leveraged OnBase to bulk-assign claims from adjuster to adjuster – or group of adjusters – as necessary. This was a revelation for MoE employees, who previously reassigned claims manually, one at a time, within the legacy system.
Before long, MoE had the solution deeply embedded within the company’s claims process. Deep enough that you might mistake OnBase for an integral piece of the core claim system rather than a supporting solution.
Enumclaw, Washington
421
Even though OnBase helped MoE extend the life of its legacy system, it soon became clear the legacy claims solution limited the insurer’s ability to extend the capabilities of OnBase. More importantly, the legacy system couldn’t keep pace with MoE’s pursuit of thoughtful customer and agent service. It was time for a new, modern core claims system: Guidewire™.
After considering its options, MoE turned to Guidewire ClaimCenter™. The insurer had experience with the solution provider, after implementing the Guidewire BillingCenter™ core system solution in 2014. The Guidewire partnership with Hyland helped seal the deal. Hyland is a Guidewire PartnerConnect™ Solution and Ready for Guidewire program member.
“The document management piece of any claims system implementation is vital,” said Obermeyer. “Inbound and outbound customer claims communication must be handled easily and efficiently if any insurer hopes to compete in our evolving industry. ClaimCenter, integrated with OnBase, fulfills that requirement.”
With ClaimCenter, MoE more accurately directs incoming documents to the appropriate claim employee, allowing the insurer to respond to customer inquiries faster. ClaimCenter more accurately and effectively pre-populates data and information for outbound correspondence and better matches it with existing documents.
— Jeff Obermeyer, claims Business Manager, Mutual of Enumclaw
Seamlessly working together, OnBase and ClaimCenter offer complete processing, intelligently linking all related information to a claim or policy and presenting it in a way most efficient to the users. With true point-and-click configuration that minimizes the need for custom coding, OnBase Solution Accelerators successfully completed the Ready for Guidewire accelerator validation process. They reduce time-to-market for new products or services, decrease capture and document management implementation time and costs by 50% or more, and improve project team performance.
Prior to implementing ClaimCenter, adjusters would jump back and forth from their legacy claims solution to OnBase. With the integration between ClaimCenter and OnBase, users work in ClaimCenter exclusively. All OnBase functionality is available to the adjuster through ClaimCenter.
Working together, the solution improves customer service throughout the claims lifecycle — from dynamic and adaptive FNOL processes that define service response to account special handling, mobile access and more.