Discovery Benefits
Insurer improves processes to meet extraordinary growth with Hyland's OnBase.
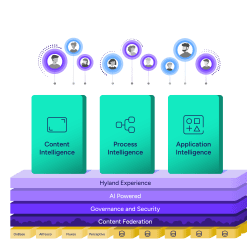
Harness the power of a unified content, process and application intelligence platform to unlock the value of enterprise content.
Learn more
Explore Hyland’s solutions by industry, department or the service you need.
Overview of solutionsIt's your unique digital evolution … but you don't have to face it alone. We understand the landscape of your industry and the unique needs of the people you serve.
 Overview of industries
Overview of industries
Countless teams and departments have transformed the way they work in accounting, HR, legal and more with Hyland solutions.
 Overview of departments
Overview of departments
We are committed to helping you maximize your technology investment so you can best serve your customers.
 Overview of services
Overview of services

Discover why Hyland is trusted by thousands of organizations worldwide.
Hear from our customers
Our exclusive partner programs combine our strengths with yours to create better experiences through content services.
Overview of partners
Find resources to power your organization's digital transformation.
Browse the resource center
Hyland connects your content and systems so you can forge stronger connections with the people who matter most.
Learn about HylandWith our modern, open and cloud-native platforms, you can build strong connections and keep evolving.
 Dig deeper
Dig deeper
Reading time minutes
Insurer improves processes to meet extraordinary growth with Hyland's OnBase.

The complex, multistep procedure for receiving, sorting and processing claims at Discovery Benefits was slow and involved too many touch points. Manual tracking and data entry required staff to pass paper forms back and forth between teams.
With a customer relationship management (CRM) tool that provided limited reporting functions, getting information to customers and managers about the status of a claim meant digging through paper files.
The company was also overwhelmed with the overtime costs associated with a manual customer renewal process each year. Leaders realized they needed to find a profitable way to grow. That's when Discovery Benefits discovered Hyland's OnBase platform.
Since deploying OnBase, Discovery Benefits has grown from providing benefits for 1.25 million people to more than 10.5 million. The company has processed more than 313 million documents into and through OnBase, with nearly 130 million still in the system. As the staff has grown from 120 to more than 800, the organization has cut out the barriers of paperwork and let employees take on more essential responsibilities — like using OnBase to review accounts electronically and discover uncollected fees.
Discovery Benefits achieved a turnaround of one business day for all claims coming into the company. Whether through fax, email, receipt upload or regular mail, information is sent via electronic forms to OnBase, where they are automatically indexed based on the claim number. Once uploaded into the system, Discovery Benefits offers customers the option of viewing their forms online so they can see the status of their claims and whether they need to follow up with more information. Discovery Benefits' staff spend far less time fielding calls from customers and searching for paperwork.
"We saved around $3 million in paper costs alone since deploying OnBase — about $500,000 a year," said Dean Johnson, OnBase senior engineer at Discovery Benefits.
And then there are the staffing costs. Before OnBase, Discovery Benefits processed 1,500 to 2,000 claims a day — about 60 to 80 per claims specialist. Currently, the provider is processing an average of 12,500 claims per day.
"This breaks down to 300 claims processed per claims specialist per day," Johnson said. "If we didn't have OnBase, we would need roughly 80 or 90 claims specialists to keep up with the incoming claim volume."
— John Biwer, President, Discovery Benefits
With 90% of Discovery Benefit’s staff in OnBase eight hours a day, the IT team has to work fast to keep up with internal process changes. Thanks to the functionality of OnBase, those are two-day projects instead of two months. Staying ahead of the speed of business is just one way Discovery Benefits has realized growth.
"Employees are always looking for a way to do something easier, quicker or better," Johnson said. "OnBase allows us to do that. There's always something we can do to make someone's job easier."
Transforming manual processes: Year-end customer renewals involved an all-paper process, with employees putting in 20+ hours a week in overtime five months out of the year. Putting the whole process into OnBase completely cut out staff overtime — and frustration — and gave them access to all renewal paperwork in a streamlined workflow.
Providing transparency: With all data centralized in OnBase, managers and supervisors run customized reports, giving them greater visibility into employees' workloads and progress. A lack of visibility used to mean weeks of digging through call logs. Now, additional training for an employee or intervention with a customer happens almost immediately.
Improving risk management: On a normal day, Discovery Benefits processes about 3,500 checks. Managing the process through OnBase allows Discovery Benefits' accounting team to instantly detect discrepancies between checks written and checks being cleared and investigate whether a check should be denied.